Request a representative visit or G7 15 Day or G7 samples
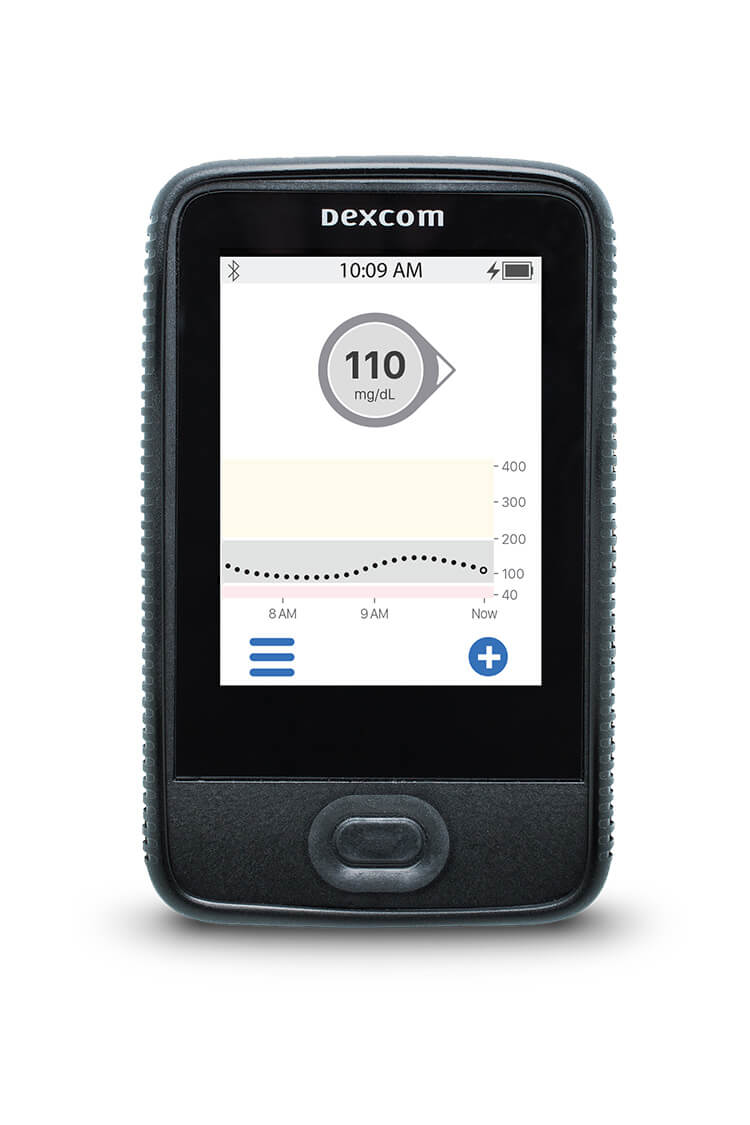
The two receivers have different hardware.* Please refer to the user guides for information about the hardware.
|
|
| Current Dexcom G6 Touchscreen Receiver | New Dexcom G6/G7 Receiver |
* Please note that images are not to scale.
The Current Dexcom G6 Touchscreen Receiver can not be upgraded to G7.
The New Dexcom G6 Touchscreen Receiver can be upgraded from G6 to G7.
Please reference Current Dexcom G6 Touchscreen Receiver user-guide here.
Please reference New Dexcom G6 Receiver user guide here.
Please reference New Dexcom G7 Receiver user guide here.
Medicare requires the use of the receiver for all patients. For all other payers, patients have the choice of what device to view their numbers. Users can also view their numbers on both their phone* and receiver if they choose.
Yes, the new Dexcom G6 receiver can be upgraded from the G6 to the G7 CGM system once your patient has a G7 prescription and has received the product. To upgrade, please instruct your patient to first use a secure internet connection to upload his/her G6 data to clarity.dexcom.com by logging in with his/her Dexcom account information and clicking Upload. Then, Clarity will ask if he/she wants to upgrade the receiver from G6 to G7. Just click the boxes to confirm that all the requirements are met. Please note that by upgrading the receiver from G6 to G7 your patient will no longer be able to use Dexcom G6 sensors or transmitters with the new Dexcom G6 receiver and your patient will not be able to revert the receiver back to G6. Your patient may opt to update from G6 to G7 any time he/she chooses, just return to Clarity and upload to be asked again.
Dexcom G6 and Dexcom G7 are available to Medicare patients through a medical distributor (see distributor list below).
Your patients may call a distributor from the list below to start the ordering process.
If your patient uses a connected insulin pump or pen,|| we recommend they continue using Dexcom G6 until our insulin delivery partners integrate with Dexcom G7.
| Distributor | Phone | Fax |
| Advanced Diabetes Supply | 877-838-3026 | 760-444-8771 |
| Byram Healthcare | 800-775-4372 | 888-457-1277 |
| CCS Medical | 800-949-6481 | 866-823-4482 |
| Diabetes Management & Supplies | 888-738-7929 | 504-734-7165 |
| Edgepark | 866-400-5183 | 866-510-6583 |
| Edwards Healthcare | 888-344-3434 | 502-657-0237 |
| Solara Medical Supplies | 800-423-0896 option 2 | 800-999-7021 |
| US Medical | 877-659-9875 | 888-659-9112 |
Medicare beneficiaries with diabetes mellitus who are using any kind of insulin will be eligible for CGMs. Frequent adjustment of insulin on the basis of CGM results is no longer required. The beneficiary must simply be insulin-treated.
For a full description of coverage criteria, Click HERE
If your patients are current G6 users, please contact your distributor for pricing and upgrading options to Dexcom G7. If your patients currently use Dexcom G6 with a connected insulin pump, we recommend continuing it until Dexcom G7 adds compatibility with your pump or pen. We're working with our insulin delivery partners to integrate with Dexcom G7 as soon as possible. Medicare covers one CGM receiver every five years.
Dexcom has a discounted receiver program through GoodRx for getting a G7 receiver at an affordable price. Visit the Dexcom Savings Center for more information. Terms and conditions apply.
Dexcom G6 and Dexcom G7 are available to Medicare patients through a medical distributor (see distributor list below).
Your patients may call a distributor from the list below to start the ordering process.
If your patient uses a connected insulin pump or pen, we recommend they continue using Dexcom G6 until our insulin delivery partners integrate with Dexcom G7.
|
Distributor |
Phone Number |
|
Advanced Diabetes Supplies |
877-838-3026 |
|
Byram Healthcare |
800-775-4372 |
|
CCS Medical |
800-949-6481 |
|
Diabetes Management & Supplies |
888-738-7929 |
|
Edgepark |
866-400-5183 |
|
Edwards Healthcare |
888-344-3434 |
|
Solara Medical Supplies |
800-423-0896 option 2 |
|
US Medical |
877-659-9875 |
No. Blood glucose monitoring (BGM) supplies are not included in the CGM product shipments because Dexcom G6 and Dexcom G7 do not require fingerstick calibrations.* Any BGM testing supplies need to be purchased.
*If your patient’s glucose alerts and readings from the Dexcom G6 or Dexcom G7 do not match symptoms or expectations, please use a blood glucose meter to make diabetes treatment decisions.
How does my patient view glucose data?
You can view your patient’s glucose data through the Dexcom G6 or Dexcom G7 Apps, your Dexcom G6 or Dexcom G7 receiver, and the Clarity Mobile or Desktop applications.
Medicare does not cover Dexcom G6 or Dexcom G7 CGM supplies that are used only with a smartphone or other mobile device. Failure to use your receiver will result in loss of Medicare coverage for your Dexcom G6 or Dexcom G7 CGM supplies.
Coverage of CGM system supplies and accessories are available for those therapeutic CGM systems where the beneficiary uses a receiver classified as DME to display glucose data. There is no Medicare benefit for supplies used with equipment that is not classified as DME. However, Medicare coverage is available for the CGM system supplies and accessories if a non-DME device (smartphone, smart watch, tablet, etc.) is used in conjunction with the durable CGM receiver. Coverage of CGM system supplies and accessories are available for those therapeutic CGM systems where the beneficiary uses a receiver classified as DME to display glucose data. If a beneficiary intends to never use a receiver classified as DME as the display device, the supplies and accessories are not covered by Medicare.
Here are some examples of how a Medicare patient may use a smart device with their receiver:
-
A patient uses both a receiver and a smartphone throughout the day
-
A patient uses a receiver some days and their smartphone other days
Patients should reach out to 1-800-MEDICARE with any questions about the Medicare coverage requirements for Dexcom CGM.
Visit www.dexcom.com/medicare to view online training videos. These videos can walk your patients through the steps to get started, including receiver and app set-up, and downloading Dexcom CLARITY
Still need help? Call Dexcom Product Education & Training to speak with a Diabetes Coach at 877-339-2664.
For technical troubleshooting, our specialists are available 24/7 at 844-607-8398.


